Clonal hematopoiesis (CH) is characterized by the somatic acquisition of malignancy associated mutations in hematopoietic stem cells (HSCs). Loss-of-function mutations in TET2 occur in one third of CH cases and are highly associated with the subsequent development of myeloid malignancies. Tet2 KO mice demonstrate increased HSC self-renewal, expansion of myeloid precursors, elevated inflammation, and progression to leukemia with long latencies, similar to CH to AML progression in humans. Additionally, leukemia development in Tet2 KO mice is dependent on increased production of pro-inflammatory cytokines such as IL-6, IL-1β, and TNF-α through hyperactive toll-like-receptor signaling (TLR). Despite extensive characterization of the adverse effects related to TET2 mutations, no effect intervention or pharmacologic therapy has been developed to slow its known progression.
To investigate altered pathways in Tet2 mutant CH that might be amenable to pharmacologic targeting, we performed RNA-seq on sorted Lin -cKIT + (LK) myeloid progenitors and Lin -cKIT +Sca-1 + (LSK) stem cells from Tet2 KO vs WT mice. We found significant upregulation of hallmark JAK/STAT3 and TNF-α signaling pathways in Tet2 KO cells. The epigenetic reader protein bromo- and extra-terminal domain 4 (Brd4) interacts with both NF-κB and STAT3 to promote transcriptional activity and regulate inflammation. We hypothesized inhibition of Brd4 would reverse abnormal hematopoiesis in Tet2 KOs via reduction in inflammatory signaling. Therefore, we generated double KO mice by intercrossing Mx1-Cre mice with Tet2 conditional KO and Brd4 conditional KO mice. While deletion of Brd4 during fetal hematopoiesis is lethal, we have successfully induced deletion of Brd4 both alone and in combination with Tet2 in young adult animals without any observed lethality for 6 months. To study pharmacologic Brd4 inhibition in Tet2 KO mice, we utilized PLX51107, a structurally distinct BET inhibitor previously reported on by our laboratory.
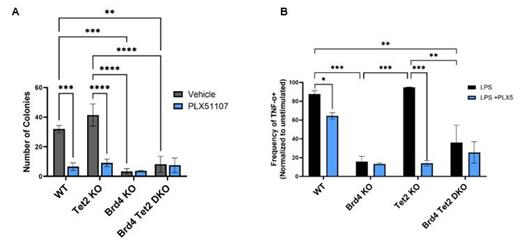
As expected, Tet2 KO marrow demonstrated increased colony formation and serial replating ability compared to WT controls. However, colony formation by Brd4 Tet2 DKO marrow was significantly decreased when compared to Tet2 KO ( p = 0.0003, n=5) or WT mice ( p = 0.0048, n=5) (Figure 1A). Similarly, PLX51107 treatment reduced Tet2 KO colony formation ( p = 0.0001, n=5) and abrogated serial replating ability ( p < 0.01, n=5). When Brd4 KO or Brd4 Tet2 DKO marrow was treated with PLX51107, which also inhibits Brd2 and Brd3, there was no significant change in colony formation compared to untreated marrow, suggesting Brd4 has a non-redundant role in colony formation. Collectively, these results suggest Brd4 plays a key role in self-renewal of Tet2 KO HSCs. To further characterize the role of Brd4 in Tet2 mutated CH, single cell RNA-seq analysis of Brd4 KO and Brd4 Tet2 DKO marrow populations is in progress.
In murine models of Tet2 CH, disease progression is associated with emergence of an aberrant population of inflammatory macrophages. We therefore investigated functional differences in macrophages from WT, single, and double KO mice. LPS-stimulated bone marrow derived macrophages (BMDMs) from Brd4 Tet2 DKO mice produced significantly less TNF-α, IL-1β, IL12p40, and IL-18 when compared to single KO or WT controls ( p < 0.001, n=3) (Figure 1B). Similarly, we found mRNA expression of these cytokines to be decreased in LPS-stimulated Brd4 Tet2 DKO BMDMs when compared to single KO and WT controls ( p < 0.001, n=3). Similar results were observed in LPS-stimulated Tet2 KO and WT BMDMs treated with PLX51107 ( p < 0.005, n=3). Additionally, PLX51107 treatment reduced protein levels pSTAT3, NLRP3, and phosphorylated p65, key downstream targets of TLR signaling, in LPS-stimulated BMDMs. Together, these results suggest that Brd4 is required for the hyperinflammation characteristic of Tet2 mutated macrophages that drive progression to myeloid malignancies.
In summary, we report that genetic or pharmacologic inhibition of Brd4 reduces the increased self-renewal and elevated inflammation in a murine model of Tet2 mutated CH. Our novel inducible double knockout mouse model of CH achieved simultaneous knockout of Brd4 and Tet2, which has never been investigated. Collectively, our data provides rationale for further pre-clinical investigation of BET inhibitors to prevent progression of Tet2 CH.
Disclosures
Larkin:Gilead: Honoraria; Debiopharm international: Research Funding; Astellas Pharma: Consultancy. Woyach:Newave: Consultancy; Loxo: Consultancy; Beigene: Consultancy; AstraZeneca: Consultancy; Abbvie: Consultancy; Schrodinger: Research Funding; Morphosys: Research Funding; Karyopharm: Research Funding; Janssen: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal